July 14, 2022
It is 2019, with repeated challenges in establishing a medical team in Florida. My google search led to an extraordinary solo practicing pain doctor, a “family” doctor. I was prepared for my first appointment as I organized a detailed folder, a book, of my medical records of medications, surgeries, procedures, etc. We were able to discuss my options candidly. Unfortunately, he felt I had exhausted the treatments available. The regimen I was on was my best option. I was reluctant and took the fentanyl refill prescription. The pharmacy was under scrutiny as the industry was regulated with a strict approval process in tracking or obtaining fentanyl patches or any opioid. The stress and stigma of opioids prescribed were at an all-time high. The daily breaking news headlined the overuse of prescription opioids and the increased overdoses of street drugs laced with fentanyl. My mind was all over the place. Were they talking about me, that middle-class woman addicted to opioids? Who do you trust? The world’s finger-pointing and judgment added a whirlwind of drama to my already complicated life. It was affecting everyone around me. My family was my motivational strength, as was my competitive drive. My genetic makeup definitely helped. A driven, stubborn ancestral history to follow. My faith was strong and will never die. I felt their presence and guidance to keep the fight.
What are my options? My pain was real. The pain was relentless, and the instability made it difficult to do daily tasks. At an appointment with my pain doctor, I insisted and begged to stop the opioids. I had been on these drugs for nine years. The ongoing stress of obtaining it and not helping the pain only made me crazy and sick. The protocol was to do a tapering-off process. I experienced headaches with flu-like symptoms with the decreased fentanyl dose. The increased pain from my elbow instability was unbearable. The wrist-twisting motion and picking up objects caused a dislocation; it felt broken. These movements aggravated the nerves in my arm. I can only describe my constant pain those days. When I moved it, I would compare it to if you ever hit your funny bone, getting that immediately intense shooting pain. I would amp it up a couple notches and add grabbing an electric fence pulsating electric shocks down your arm. I called them zingers. It was apparent it was anatomical and not drug dependence. It was the first time the thought of amputating came to mind. I contacted my Michigan surgeon; he recommended a revised elbow replacement before considering amputation. Since he was out of network with my insurance, I had to find an orthopedic in my network. The Florida surgeon said my elbow was complex and out of his expertise. He had no alternative except was advised to continue pain management.
It was bizarre to me that I was unfixable. I will not accept and will not spend my days in this pain and feel like a criminal. Every month the same bull…sh,. I continued to taper off the fentanyl patch. It was an overwhelming battle dealing with the withdrawal, increased pain, and filling the prescriptions at the pharmacy. I had to call or drive around each pharmacy in the area; no one could guarantee availability. Many pharmacists wouldn’t discuss anything regarding opioids; a handful directed me to a pharmacy that could. The looks were, with disgust, as another, with pity; both saw me as a drug addict.
I was stuck on the same roller coaster with the internal emotions and physical battles. One day asking myself, is this all in my head? The bouts of frustration and anger, the why me in a dark room alone. The next day, on the floor in intense pain, with nowhere to go to get relief. My status in the medical community no longer filed as “no man’s land,” I was flagged as a drug seeker.
On May 20th, 2019, I met up with friends to play tennis. I had played at least weekly for a year, but it was hit or miss lately; coming off the medications and increased pain was exhausting. I needed socialization and competitive endorphins to give me a boost. We were finishing up a game when someone suggested playing longer. I hesitated a second, but my competitiveness pushed on. I went for an overhead hit at the baseline, took too many steps back, and fell on my left hand onto the racquet. The force caused my wrist into the palm of my hand, a definite fracture. My hand and wrist were in a deformed configuration. I was in shock with adrenaline as I continued to pick up the ball and walk over to my bag. My friends were also shocked and expressed the immediate need to be taken to the hospital. On route, reality and pain set in. An x-ray confirmed the obvious. It was set in place and then sent to a hand surgeon. Two days later, surgery to stabilize the radius fracture with a plate and screws. After two weeks in a surgical cast, sutures were removed into a fiberglass cast for four weeks. The fiberglass cast was removed, then onto physical therapy. I rehabilitated great, except my emotional state was maxed out.

The physical activities were a comedy of errors and a learning curve to do anything. I am surprised I wasn’t admitted to a padded room. The limitations of both arms, the right arm worse each day with the double duty required to use while the other arm healed. Too much time with no hands had my nose into the computer doing extensive online research; I read a few great articles written by a top orthopedic elbow surgeon at the Mayo Clinic in Rochester. Ironically, my insurance was in-network there. I emailed a detailed summary of my medical records to Dr. Shawn O’Driscoll. He responded immediately. We did a zoom meeting to further discuss if he could help. We agreed to further the evaluation in person. He determined the artificial prosthetic had loosened, and the radial attachment had shifted out of place. My surgery was scheduled for October 30th, 2019, for a revised total elbow replacement with exploratory of the ulnar nerve.
My strategy was to be entirely off the fentanyl patch before surgery. My pain doctor was adamant about dropping too fast. I asked if it would kill me. He said no, I would have uncomfortable withdrawal symptoms. The duration and dosage of the fentanyl patch I had been on for several years; the protocol was to taper over several months by increments of 12.5 mcg to 25 mcg. I was down 25 mcg in a month. I went cold turkey, 50 mcg to zero in a day. I am the type who pulls the bandaid off quick versus slow. My goal was to detox my body to prepare for the surgery scheduled in a month and a half. Let me just say, I wouldn’t wish my worst enemy to go through this withdrawal process. Fortunately, I was solo those days. I wanted it that way. I will spare the details. I am glad I did it and will never go through that experience again.

On surgery day, I was a tad under the weather. My body was still adapting and adjusting after nine years of opioids and cocktails of medications. I was mentally prepared for surgery as I felt my body’s challenge was also from the pain. Dr. O’Driscoll performed the surgery; he replaced the elbow component and elected to leave out the radial head component. In his experience, the revised radial head on a revised total elbow has complications and a low success rate. The ulnar nerve was a zig-zag, impossible to distinguish, which added to his decision. The hope was the soft tissue would support the radial bone. He expressed guarded optimism about my prognosis.

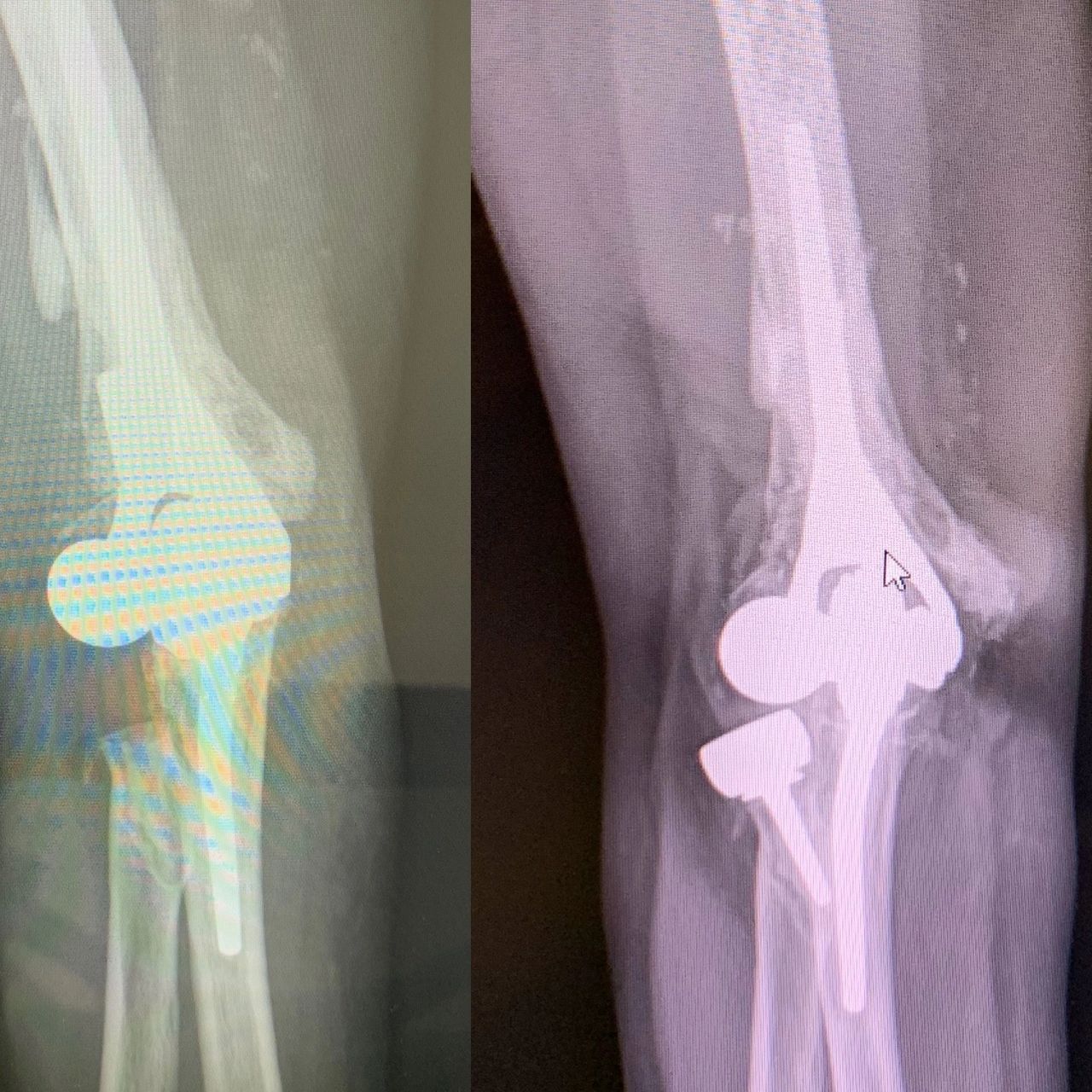
I flew home two days later in an enormous heavy surgical cast, fixed straight and as big as my leg. I established a good relationship with my hand surgeon instead of flying back to Rochester for my 2-week post-op. Dr. Chan agreed to take the x-rays and remove the cast and sutures for Dr. O’Driscoll. At the same appointment, we discussed the removal of the wrist hardware. The friction of the metal was causing irritation to a tendon that made my middle finger stick, called a trigger finger. He injected a steroid for the inflammation. The surgery would be scheduled at a future date to allow the other arm to heal. One hand at a time.


