April 24, 2022
Six weeks was a long healing process on the machine. I fought an infection at the surgical site, taking numerous medications with high doses of antibiotics. In a zombie state, I sat in a zero gravity chair my girlfriend lent to me to be comfortable while the machine did its work by my side. I slept on the trundle bed in the guest room. The noise of the machine kept Jeff from sleeping. He needed his sleep as he carried the load of the whole household, his demanding job, and caring for me. He would drive back and forth from work a couple of times a day during his busiest time of year. On four occasions, he was stopped for speeding. He would apologize to the officer as he explained our situation. At the fourth stop, he received a ticket. He was going 90 mph in a 55 mph zone. He worked 30 miles away, 25 miles was open farm country with no stoplights. The biggest obstacle was encountering deer. It was a 45-minute drive one way. My friends helped drive Zack to his afterschool activities. My daughter returned home from college to recover from a broken foot. We concurred and survived. I have no idea how. I was finally relieved of the machine. The elbow was healing great. I started physical therapy. It progressively aggravated and caused enormous pain to my shoulder and my arm. I tried to push through it, the no pain no gain theory. At one of the physical therapy sessions, my arm went completely limp. It turned several shades of blue and purple. The muscle spasms were so bad. It jerked my head and neck. The hand surgeon in the building witnessed this reaction. He made his assessment and called my doctor. Both agreed I should try injections called stellate ganglion blocks. This procedure injects pain medication directly into the nerves of your spine. The idea was to calm the nerves going down my arm to help the healing of my brachial plexus nerve injury.
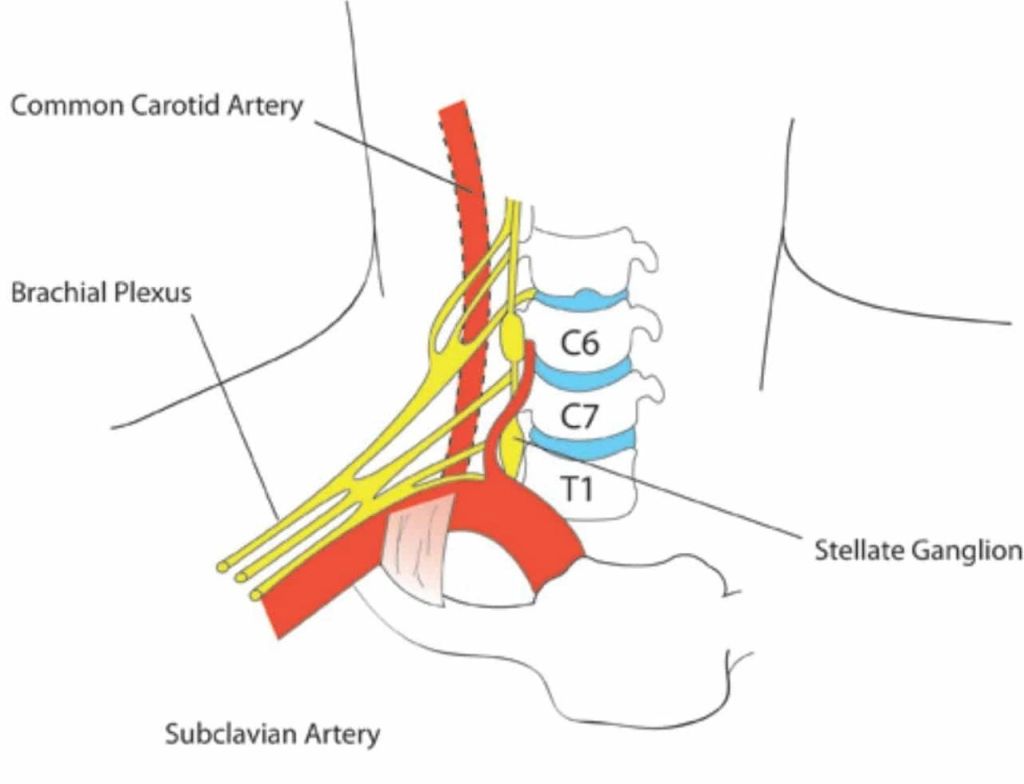
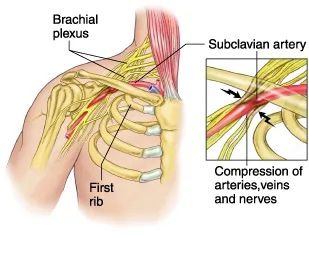
The protocol was at least three injections to benefit from the procedure. The first injection helped for an hour but gradually returned. The second injection increased the pain and made the spasms more constant. On the third injection, the nurse was prepping me for the procedure. The spasms were so intense that she had difficulty as I shook on the table, embarrassed I could not control it. She requested the doctor to get his advice. I remember him telling her in an egoistic response with no empathy. He said, no worries, once we give anesthesia. She will be fine. It did not help, as the spasms and pain were nonstop. At my follow-up EMG, the spasms were so bad. The doctor decided to inject botox to calm them. It helped immediately. On my next visit, I had a couple of areas where she injected more Botox. This time by the time I got home. I could not swallow while my voice went hoarse. I called the doctor immediately. I was scared. It was like I had no control. The feeling after your mouth is numb for a tooth retraction but in my throat. It was primarily on the right side. She was concerned and had me return immediately to her office. Her explanation was she was more aggressive in this session, hoping this would eliminate the spasms. She referred me to a swallow specialist to teach me how to swallow due to the right side paralzed muscle. So I did not choke while the botox wore out. The good news is I had no spasms. In about 8 weeks, I was back to eating. In the meantime, Dr. Chouinard was happy with the elbow healing. My range of motion was almost perfect. He decided to address the shoulder. I had a CT scan that showed I had damage he could fix with surgery. It would mean I would be in a restricted sling for 2 months. Until the elbow could completely heal, he did an injection to the shoulder to help with inflammation and pain. As the elbow healed he referred me for a consultation on my brachial plexus injury. My latest EMG still showed damage and with the unsuccessful blocks. It was time to address. Dr. Quinn specialized in brachial plexus injuries. He recommended I have surgery to release the brachial plexus at the shoulder. He called it thoracic outlet syndrome. The horse to tree impact caused a compression between the collarbone and first rib. The surgery is called a transaxillary first rib resection, taking out the first rib that will provide space and relief to the nerves down my arm. I had the surgery in May 2011. He felt it was a success as the plexus was extremely compressed. It will take time to heal and calm the nerves. I was referred to Dr. Jones, for pain management. I tried several different sedatives, stimulants, narcotics, GABA, and antidepressant medications. I found nothing helpful, only many horrible side effects. He suggested a patch called Fentanyl. When the patch was first applied it worked great on the third day, the pain was intense and magnified. I had good days and bad days. On the bad days, the pain felt like a vice clamped down as hard as it could from my shoulder to my hand with zingers zapping me like an electrical pulse. If you ever touched an electric fence, it was similar but stronger as it never eased up. My whole arm was blue and red felt like a bad burn. My bad days. I would flip-flop around in bed in agony, trying to fall asleep to escape the pain. On my good days, I took advantage of life. I looked fine and healthy other than my hand worked like a claw and was a tad different from the other hand to the muscle atrophy from nerve damage. Dr. Jones increased the dosage and prescribed it every other day plus an opioid called Norco for breakthrough pain and Flexeril for sleep. I was on this regimen for a while. It seemed to work. I even rode Kommander for a few rides around the barn property. I had some normalcy. Dr. Chouinard is still concerned with the nerve damage from the updated EMG. It showed improvement with the brachial plexus with no improvement with the damage at the elbow. He referred me to a hand specialist. Dr. Leslie’s evaluation determined the damage was not a surgical option. It had been too long. If I had surgery now, I would lose all of my hand function. I had the function of my thumb and index finger, I called it my pincher. He did feel I had a condition called CRPS II, complex regional pain syndrome II. A neurological condition caused by nerve damage. It is considered the worst pain in the medical community. He referred me to a specialist at Cleveland Clinic for an evaluation. It is a difficult disorder to diagnose, treat and control the pain.
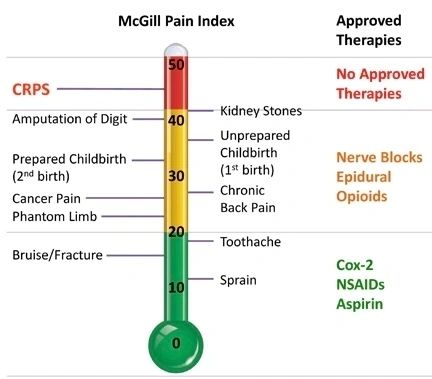
Cleveland Clinic was on the cutting edge with treatment. Jeff took me and drove the 7 hr drive one way. The doctor asked questions about my symptoms, looked at my arm as there were no tests to officially diagnose this disorder. He had two available options. The first was a spinal stimulator. This procedure implants a rod in your spine to give electrical impulses to interfere with the pain message that the nerve was sending to the brain. The rod would be implanted into my neck. In this placement, most patients had complications of it migrating from the movement of the neck. It was also more successful with patients relieved from the stellate ganglion blocks, which I did not get. The other option and highly recommended by this doctor was a ketamine coma. You are in a supervised induced coma for 5 days. The idea is it would reprogram the brain from perceiving the pain. It was not approved or covered by insurance and cost over $100,000. As I researched, the studies lacked positive feedback on being successful, many with long-term side effects. I was skeptical that I even had CRPS II. I was exhausted and overwhelmed from all the different doctor appointments with their pokes, probs, surgeries, and medications. Could it be that my body just needs time to heal?
